Aortic Dissection Malpractice
One of the most recurrent types of cases that our malpractice attorneys have handled involves a failure on the part of a doctor to timely diagnose a patient with an aortic dissection and/or ensure that the patient undergoes emergent cardiothoracic surgery to repair the dissection prior to its rupture and the inevitable death of the patient.
These cases are always extraordinarily tragic because the patient’s life almost always hangs in the balance where the difference between life and death is incredibly timely and urgent. According to the Smidt Heart Institute at Cedars-Sinai, “the mortality rate for an aortic dissection is about 1% an hour for the first 48 hours.” Having diligent care is essential to surviving a condition of this immediacy.
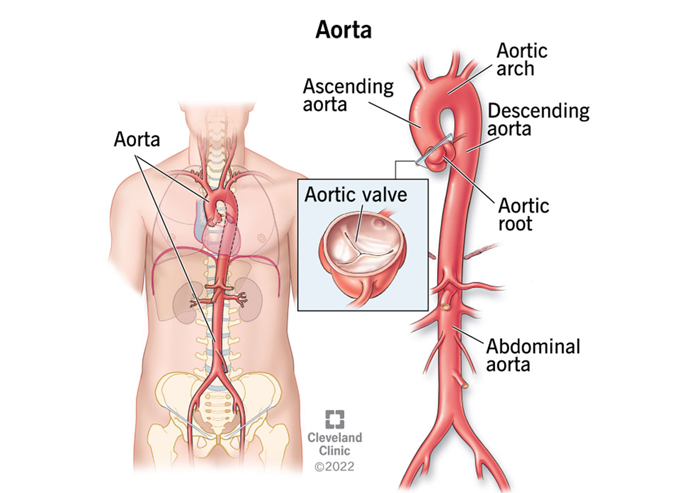
Understanding the Anatomy of the Aorta
The aorta is the large vessel that comes out of the heart that is shaped like a candy cane and delivers oxygen-rich blood to the body. The portion that is closest to the heart is the ascending aorta, which leads to the “arch” as the aorta curves around to the descending portion of the aorta. The descending aorta drops all the way down into the abdomen where it connects to various other blood vessels.
Think of the aorta like a pipe with three layers:
- The inner most layer of tissue is called the intima: the tube through which blood passes to transport oxygen and nutrients.
- The middle layer of tissue is called the media: a layer made up of smooth muscle tissue that widens and narrows to meet the body’s blood flow needs.
- The outermost layer of tissue is the adventitia: the layer that anchors the aorta in place and connects it to nerves and tissue.
Read more about the aorta’s anatomy and function from the Cleveland Clinic.
How Does an Aortic Dissection Occur?
There are several reasons why an aortic dissection may occur. Some people have fibromuscular dysplasia (FMD) which is a rare blood vessel condition that causes them to develop a weakness in the intima layer over time. In people who have long-standing/chronic hypertension (high blood pressure), the force of the blood through the aorta results in an area of weakness in the intima. This weakness, in turn, leads to erosion of an area of intima. The erosion results in a small tear and separation (dissection) of the inner most lawyer and the middle layer of the aorta creating what is called a “false lumen” (a false passageway for the blood).
Because blood is being continually pumped through the aorta, some of the blood will naturally flow into this small tear/false passageway for which there is no exit. Pressure builds up as a result. As the blood-filled channel gets bigger and larger, eventually the pressure becomes too great and the aortic wall ruptures, resulting in a catastrophic loss of blood into the area around the heart chamber. This loss of blood causes other organs to be deprived of the necessary oxygen rich blood and can fill the heart chamber to the point where it compresses the heart and impedes its ability to beat. Because it is a life-threatening condition, it must be recognized and treated as quickly as possible.
Identifying an Aortic Dissection
Health care providers are taught to recognize the hallmark signs and symptoms of an aortic dissection so that it can be treated prior to rupture. If diagnosed timely, aortic dissections are either repairable surgically or medically, depending on the location of the tear. As we previously stated, in most instances, survivability can change (greatly enhanced) from hour to hour.
So, what are the typical signs and symptoms of an aortic dissection? A brief list includes:
- Shortness of breath;
- Severe chest or back pain: patients often have described the pain as stabbing, tearing or ripping in nature;
- Fainting or dizziness;
- Low blood pressure;
- Heart murmur;
- Rapid weak pulse
- Heavy sweating;
- Loss of vision;
- Sudden presence of weakness or paralysis; or
- Loss of consciousness.
Perhaps the most important symptom is the description of the pain. Whenever a patient comes into an emergency room with a complaint of severe chest pain, health care providers should attempt to rule out the three potentially imminently fatal diagnoses that are characterized by severe chest pain: (a) heart attack; (b) pulmonary embolism; and (c) aortic dissection.
Thus, aortic dissection should never be far from a physician’s mind when a patient is complaining of severe chest pain. Whereas a heart attack is typically ruled out by certain blood tests and/or an EKG, an aortic dissection and pulmonary embolism can only be ruled out by employing various radiological studies like ultrasound, CT scan, and MRI.
For an aortic dissection, the first diagnostic step that physicians should normally take is to order a transthoracic echocardiogram (TTE). This is a test that utilizes sound waves to create an image of the heart from outside the body.
A TTE, however, has limitations and thus doctors will, if there is any doubt, order more sensitive radiological studies such as a CT angiogram (with dye), an MRI, or a transesophageal echocardiogram (TEE) (a study in which a tiny camera is dropped down the patient’s esophagus near the heart and aorta to see if there is a tear in the aorta. Comparatively, the CT angiogram and MRI are less invasive. The CT angiogram uses x-rays to give doctors a cross-sectional view of the body after the contrast dye illuminates the heart and artery. The MRI is used to make pictures of the aorta using magnetic fields and radio wave energy. The TEE, CTA and MRI area are generally seen as more sensitive and better diagnostic tools than the TTE.
Read more about diagnosing aortic dissection here.
What Happens if a Tear and False Lumen Are Identified in the Aorta?
As mentioned above, the treatment depends on the location of the tear. If the aorta has a tear in the ascending aorta or the arch, this is what is known as a Type A dissection (most common and most dangerous). The treatment is almost always urgent surgical repair. In many cases, patients are life-flighted by helicopter to heart centers that have cardio-thoracic surgeons who have the necessary skill and experience to perform this type of surgery.
By contrast, if the tear happens in the descending aorta traveling away from the heart, it is called a Type B dissection, and the treatment is often to treat the tear medically with medications like beta blockers to reduce the heart rate and lower the blood pressure to prevent the dissection from getting bigger. In some cases, however, surgical repair of the descending aorta is still necessary.
Read more about type A vs. type B aortic dissections here.
Contact an Experienced Medical Malpractice Attorney
At Silverman Thompson, our attorneys have successfully handled many cases in which doctors have negligently failed to timely diagnose or treat aortic dissection. In many instances, patients’ lives could have been saved had doctors suspected aortic dissection and transferred the patient to a facility that could perform the surgery emergently. For example, in one case, a man was diagnosed with a possible aortic dissection but not transferred to a facility that could have saved his life for over 20 hours. He died in the helicopter on the way to that hospital. In another case, physicians negligently ignored the signs and symptoms of a clear aortic dissection in a young woman over a period of 9-10 hours. Ultimately, her dissection ruptured and she died without treatment.
Read more about Silverman Thompson’s work in cardiology malpractice here.
If you or a loved one has been affected by aortic dissection malpractice, it is critical to have an informed, detail-oriented, and dedicated medical malpractice attorney who will tirelessly advocate for you and your case. Please contact Andrew G. Slutkin and Ethan S. Nochumowitz for a free consultation at 800-385-2243.






